- Intended for US Audiences Only
- Important Safety Information
- Prescribing Information
- Information for Patients
- For Healthcare Professionals

to a maintenance
therapy with
options
Personalized CIDP maintenance therapy
You’ve got options! HyQvia can provide different ways to get your treatment. You and your doctor
can find the right combination to create an infusion experience that’s best for you.
HyQvia allows you to get your IG + Hy:
Every 2, 3, or 4
weeks as prescribed
by your doctor
Through 1-3
infusion sites*
In the abdomen
or the thighs
At home or in an
infusion center
With the support of
a healthcare provider,
or through self-infusion
with the help of a
care partner after
appropriate training
*If using three sites, the maximum is 400 mL per site.
Here are some things to keep in mind:
- Don’t be surprised by the amount you infuse. It’s a large volume. Remember when we went over Hy? Well, Hy is what helps your body handle this larger volume: ~5 cups (1200 mL, or 600 mL for people weighing <40 kg [88 lbs]) is the most you’d infuse in a day. Thus, you’ll go through a ramp-up period to help you get used to this amount
- It’s common to need more than one infusion site to receive your full dose. Most patients infuse using 2 sites, but because administration can be adapted to fit your needs, you might use only 1 site or could even use up to 3 sites. If you weigh 40 kg (88 lbs) or more, the maximum infusion volume is 600 mL per site (or as tolerated); if using three sites, the maximum is 400 mL per site
- While many people are able to receive their full dose in one infusion, you may need to split your dose over more than one day

When learning about
an IG therapy for CIDP,
it’s important to consider
your infusion preferences,
including how and where
you infuse.
Multiple site of care options
HyQvia can be administered across multiple sites of care, including hospitals, infusion
centers, offices, or at home with the support of a healthcare professional. Appropriate
training is required prior to self-infusion.
In-center
HCP-supported administration might be the way to go if you:
- Are not comfortable or unable to self-administer
- Are apprehensive of or fear needles
- Prefer infusions to be handled by a HCP
- Lack the organizational skill, dexterity, or drive to reliably self-administer
At home
You might prefer self-infusion after appropriate training or HCP- or caregiver-supported administration if you:
- Have logistical issues attending or live far away from an infusion center or a clinic
- Need to fit infusions around work/home life
- Want more independence with the option to self-infuse at home or an alternate location after appropriate training
- Want an option that simplifies the at-home infusion process with fewer steps and supplies using HyHub

Introducing HyHub
HyHubTM and HyHubTM Duo are two single-use infusion trays for patients 17+ with Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) as prescribed. These trays are designed to simplify infusion preparation by reducing the number of steps, when using 2-4 dual vial units (DVUs), to prepare Hy and IG compared with a pooling bag. Have questions? Check out the FAQ for more details on HyHub or download the Step-by-Step Infusion Guide.
HyHub/HyHub Duo Important Information for Patients
What is HyHub/HyHub Duo? HyHub/HyHub Duo are stand-alone, single-use, disposable vial access devices.
Who Should Use HyHub/HyHub Duo? HyHub/HyHub Duo are for patients 17 years of age and older to allow HyQvia to be transferred from vials without using a needle, as prescribed, in a home environment or clinical setting.
Do Not:
- Use HyHub/HyHub Duo with a pooling bag.
- Connect HyHub/HyHub Duo to a syringe driver infusion pump.
Selected Information for Patients:
- HyHub/HyHub Duo are for SINGLE USE ONLY, even if all docks are not used during a single infusion. Re-use will increase risk of infection. Always use a new HyHub/HyHub Duo for each infusion.
- Only use HyHub/HyHub Duo when ready to administer HyQvia.
- Do not use HyHub/HyHub Duo at home until receiving instructions and training from a healthcare provider.
- HyQvia is the only medicine that may be used with HyHub/HyHub Duo.
- Do not exceed the maximum infusion volume per infusion site or infusion rate as indicated in the HyQvia prescribing information, or as directed by a healthcare provider.
For safe and proper use of HyHub/HyHub Duo, please refer to the complete Instructions for Use included with the devices. Talk to your healthcare provider if you have additional questions. For information about HyQvia, including warnings for blood clots, please see Patient Information for HyQvia.
Considering HyQvia?
Watch this video to find out if HyQvia might be an option for you.
Nurse: What is HyQvia?
HyQvia is a liquid medicine that is given under the skin (subcutaneously) to treat chronic inflammatory demyelinating polyneuropathy (CIDP) in adults.
IMPORTANT SAFETY INFORMATION
What is the most important information that I should know about HyQvia?
- HyQvia can cause blood clots.
- Call your healthcare professional (HCP) if you have pain, swelling, warmth, redness, or a lump in your legs or arms, other than at the infusion site(s), unexplained shortness of breath, chest pain or discomfort that worsens on deep breathing, unexplained rapid pulse, numbness or weakness on one side of the body.
- Your HCP may perform blood tests regularly to check your IgG level.
- Do not infuse HyQvia into or around an infected or red swollen area because it can cause infection to spread.
Nurse: Please see Important Safety Information throughout this video, and accompanying Information for Patients, including Warning about Blood Clots, or visit www.hyqvia.com/information-for-patients.
Nurse: Hi, and welcome! My name is Rachel, and I’m a nurse. I’m here to tell you about HyQvia, a treatment that can be used as a maintenance therapy for adults with CIDP. We’re going to briefly go over what HyQvia is and how it works.
Nurse: HyQvia is the unique combination of IG with hyaluronidase
HyQvia is a CIDP maintenance therapy that can meet you where you are
HyQvia can be administered across multiple sites of care, including hospitals, infusion centers, offices, or at home, whether it’s self-infused after appropriate training, or with the support of a healthcare professional or care partner.
Nurse: But first, what is CIDP?
Nurse: CIDP stands for chronic inflammatory demyelinating polyneuropathy, an autoimmune disorder that may get worse over time.
People who have CIDP are believed to have an autoimmune disease in which the body's immune system targets the nerves, leading to muscle weakness and numbness, usually in the arms and legs.
Nurse: So, what makes HyQvia different?
Nurse: Hyaluronidase, or Hy, which can be found in your body naturally.
Hy is the first part of your infusion, and it allows a larger amount of IG to be absorbed into your subcutaneous tissue – a layer of tissue under your skin – and then into your bloodstream. This is how you’re able to infuse every 2, 3, or 4 weeks as prescribed by your doctor.
Nurse: Don’t use HyQvia if you’ve had a severe reaction to IG, hyaluronidase, other blood products, or any ingredient in HyQvia.
Nurse: When it comes to getting your CIDP maintenance treatment, HyQvia may provide you with choices for your infusion experience.
HyQvia offers you the option for your treatment to be given at an infusion center or at home with the help of a nurse, or even by yourself after appropriate training.
Nurse: And along the way, you can change where you get your infusions. For example, you could start at the infusion center and then have an infusion nurse come to your house and help with your infusions. Or, after you or your caregiver have received instruction and appropriate training from your HCP, you can do it without a nurse. Always talk with your doctor about which option might work best for you.
Nurse: Whichever location you choose, HyQvia is infused subcutaneously, or the subQ way, meaning it’s given under your skin rather than into a vein.
So, no IV.
Nurse: HyQvia, a liquid medicine, is the only combination of IG + Hy that has up to monthly infusions, every 2, 3, or 4 weeks.
So HyQvia could allow you to go up to 28 days between infusions, as prescribed by your doctor, based on administration every 2 to 4 weeks.
Which may give you time for the things you enjoy.
Nurse: Now, in a study, the average infusion time to deliver the monthly HyQvia dose is about 2 hours, and there is also travel time to and from the infusion center to consider.
Nurse: HyQvia can make live viral vaccines not work as well for you. Talk to your doctor before you get any vaccines while you are taking HyQvia.
Nurse: Tell your HCP if you:
- Have or had any kidney, liver, or heart problems or history of blood clots because HyQvia can make these problems worse.
- Have IgA deficiency or a history of severe allergic reactions to IgG or other blood products.
- Are pregnant, trying to become pregnant or are breast feeding. It is not known whether HyQvia can harm the unborn baby or breastfed infant.
Nurse: There’s a free trial program called HelloHYQVIA that can help you and your doctor determine if HyQvia is right for you.
With HelloHYQVIA, eligible patients will receive training with a nurse, access to a step-by-step video that walks you through the infusion process, and access to multiple resources. Talk to your doctor and visit HyQvia.com to learn more.
Nurse: If you’re interested in co-pay support, Takeda Patient Support Co-Pay Assistance Program can cover up to [100%] of your out-of-pocket co-pay costs, if you're eligible.*
To learn more, visit TakedaPatientSupport.com or call our support specialists at 1-866-861-1750.
Nurse: All of us behind HyQvia want to see you succeed.
Ask your doctor about HyQvia, and you can always visit HyQvia.com to learn more.
Nurse: There’s even a doctor discussion guide on the website to help you navigate the conversation with your doctor. You’ll see me again in the infusion video if you and your doctor decide HyQvia is right for you.
Nurse: Hope to see you there.
Nurse: What is HyQvia?
HyQvia is a liquid medicine that is given under the skin (subcutaneously) to treat chronic inflammatory demyelinating polyneuropathy (CIDP) in adults.
IMPORTANT SAFETY INFORMATION
What is the most important information that I should know about HyQvia?
- HyQvia can cause blood clots.
- Call your healthcare professional (HCP) if you have pain, swelling, warmth, redness, or a lump in your legs or arms, other than at the infusion site(s), unexplained shortness of breath, chest pain or discomfort that worsens on deep breathing, unexplained rapid pulse, numbness or weakness on one side of the body.
- Your HCP may perform blood tests regularly to check your IgG level.
- Do not infuse HyQvia into or around an infected or red swollen area because it can cause infection to spread.
Nurse: Who should not take HyQvia?
Do not take HyQvia if you:
- Are allergic to IgG, hyaluronidase, other blood products, or any ingredient in HyQvia.
Nurse: What should I avoid while taking HyQvia?
- HyQvia can make vaccines (like measles/mumps/rubella or chickenpox vaccines) not work as well for you. Before you get any vaccines, tell your HCP that you take HyQvia. What should I tell my HCP before I start using or while using HyQvia?
Tell your HCP if you:
- Have or had any kidney, liver, or heart problems or history of blood clots because HyQvia can make these problems worse.
- Have IgA deficiency or a history of severe allergic reactions to IgG or other blood products.
- Are pregnant, trying to become pregnant or are breast feeding. It is not known whether HyQvia can harm the unborn baby or breastfed infant.
Nurse: What are the possible or reasonably likely side effects of HyQvia?
HyQvia can cause serious side effects. If any of the following problems occur after starting HyQvia, stop the infusion immediately and contact your HCP or call emergency services:
- Hives, swelling in the mouth or throat, itching, trouble breathing, wheezing, fainting or dizziness. These could be signs of a serious allergic reaction.
- Bad headache with nausea, vomiting, stiff neck, fever, and sensitivity to light. These could be signs of irritation and swelling of the lining around your brain.
- Reduced urination, sudden weight gain, or swelling in your legs. These could be signs of a kidney problem.
- Pain, swelling, warmth, redness, or a lump in your legs or arms, other than at the infusion site(s). These could be signs of a blood clot.
- Brown or red urine, fast heart rate, yellow skin or eyes. These could be signs of a liver or blood problem.
- Chest pain or trouble breathing, blue lips or extremities. These could be signs of a serious heart or lung problem.
- Fever over 100°F. This could be a sign of an infection.
Nurse: After HyQvia infusion a temporary, soft swelling may occur around the infusion site, which may last 1 to 3 days, due to the volume of fluid infused.
The following possible side effects may occur at the site of infusion and generally go away within a few hours, and are less likely after the first few infusions.
- Mild or moderate pain
- Redness
- Swelling
- Itching
The most common side effects of HyQvia are:
- Headache
- Fatigue
- Nausea
- Fever
- Itching
- Redness
- Abdominal pain
- Back pain
- Pain in extremity
Antibodies to the hyaluronidase component of HyQvia were formed in some patients taking HyQvia. It is not known if there is any long-term effect. In theory, these antibodies could react with your body’s own hyaluronidase (PH20). PH20 is present in the male reproductive tract. So far, these antibodies have not been associated with increased or new side-effects.
Nurse: These are not all the possible side effects. Talk to your HCP about any side effect that bothers you or that does not go away.
Please see Important Safety Information throughout this video, and accompanying Information for Patients, including Warning about Blood Clots, or visit www.hyqvia.com/information-for-patients.
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch, or call 1-800-FDA-1088.
Ramping up when starting treatment
There’s an adjustment period when starting HyQvia to help your body get used to
treatment.
With HyQvia, you’ll go through something called a “ramp-up” period. What that means is
you’ll start with a lower amount of HyQvia and slowly increase until you reach your full
dose. There are different approaches to ramping up your dose—each approach takes
multiple weeks. You’ll work closely with your doctor to choose the right ramp-up
experience for you based on your dosing interval.
A ramp-up period doesn’t happen overnight
For example, you’ll start with infusing 25% of your monthly dose your doctor has prescribed and will slowly increase each time you infuse until you reach the full amount. Some weeks, you may skip an infusion and won’t receive any HyQvia at all.
The charts below are only examples of how your HyQvia dose may be ramped up. The percentages shown are based on the monthly calculated maintenance dose (targeted every 2, 3, or 4 weeks). Be sure to always take HyQvia as prescribed by your healthcare professional.
Dose ramp-up schedule if you will be receiving your maintenance dose every 2 weeks
X=No ramp-up infusion.
Dose ramp-up schedule if you will be receiving your maintenance dose every 3 weeks
X=No ramp-up infusion.
Dose ramp-up schedule if you will be receiving your maintenance dose every 4 weeks
X=No ramp-up infusion.
After the infusion
You may have a soft, wide swollen area around your infusion site due to the amount of fluid
you infused. It’s called a “pancake,” and it’s normal! It means Hy worked and is helping the
IG disperse in your fatty tissue. It should go away after 1-3 days.
Before infusion

End of infusion

1-3 days after infusion
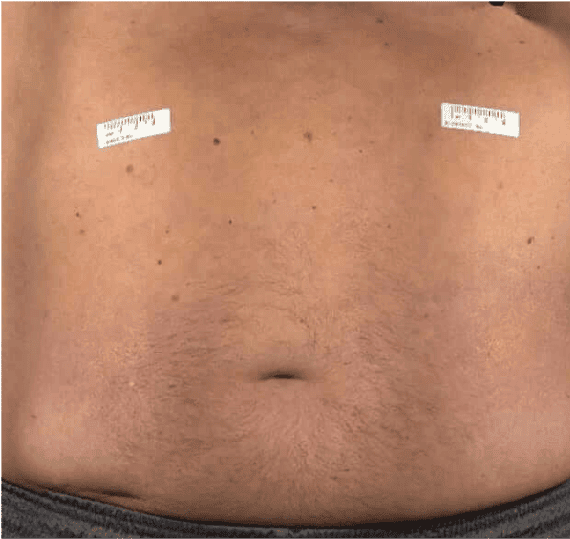
Images are of a patient from a CIDP clinical trial who had 640 mL of HyQvia infused, divided into two sites.
Say Hy to infusing HyQvia
Watch the videos below to see a nurse walk through the infusion process at home and see a nurse walk
through the infusion process using HyHub.
Videos
Transcript
Say Hy to Hy5 Video

Say Hy to HyHub With Peristaltic Pump Video
Nurse: What is HyQvia?
HyQvia is a liquid medicine that is given under the skin (subcutaneously) to treat chronic inflammatory demyelinating polyneuropathy (CIDP) in adults.
IMPORTANT SAFETY INFORMATION
What is the most important information that I should know about HyQvia?
- HyQvia can cause blood clots.
- Call your healthcare professional (HCP) if you have pain, swelling, warmth, redness, or a lump in your legs or arms, other than at the infusion site(s), unexplained shortness of breath, chest pain or discomfort that worsens on deep breathing, unexplained rapid pulse, numbness or weakness on one side of the body.
- Your HCP may perform blood tests regularly to check your IgG level.
- Do not infuse HyQvia into or around an infected or red swollen area because it can cause infection to spread.
Please see Important Safety Information throughout this video, and accompanying Information for Patients, including Warning about Blood Clots, or visit www.hyqvia.com/information-for-patients.
Nurse: Hi! I’m Rachel, and I’m a nurse. I’m here with Steve to help him learn how to self-infuse HyQvia, which just means after he’s trained correctly, he’ll be able to infuse at home by himself.
So, Steve, just so you know, if you wanted to have a family member or a friend help because of any dexterity limitations, like it’s hard or awkward to reach somewhere, all the steps I’m going to walk you through stay the same.
Patient: OK.
Nurse: Are you ready?
Patient: I think so. I’m a little nervous.
Nurse: That’s normal. I’m going to walk you through everything. And with proper training, you will be able to do this. So, I see you’ve got some supplies here. Since you’re infusing at home, the specialty pharmacy likes to make sure you have everything you need ahead of time.
Each person’s supplies may look different from the ones shown here.
Is this all they sent you?
Patient: Yeah, I think that’s everything. It’s…a lot.
Nurse: I know. It IS a lot, and I’m sure it was a bit overwhelming looking at all of this for the first time, but that’s why I’m here. It’ll all make sense.
Remember to always reach out to your doctor if you have questions or concerns.
Nurse: Let’s start with the obvious. Here are your HyQvia vials. The number of vials each person will have will depend on their dose. This guy’s your pump with power supply and its tubing. You’ve got an IV pole and syringe. This is your pooling bag and tubing. There’s your sharps container. This is what you put things in, like your needles, to dispose of when you’re done. We’ll get to that at the end of the infusion. And you’ve got an infusion mat and a Wellness Journal here. These help you organize your supplies and then track your treatments, any reactions, and has space to write down any notes or questions. We’ll get to this at the end of your infusion, too.
Nurse: OK, these are your gloves, obviously. You’ll wear these if your doctor recommends that you should. There’s a bag of saline solution, needle, or needle-less transfer device, one per Hy vial, needle set, tape, bandages, and alcohol swabs to clean the tops of your vials and your body where you infuse.
Nurse: I just said a ton, and I can see the look on your face. What are you thinking?
Patient: Well, that’s…so much, but I think I caught most of it.
Nurse: I understand. I know it’s a lot. You’ll start to remember everything. So, now that we know you’ve got everything, ready to get started?
Patient: I’m a little nervous, but let’s do it.
Nurse: Great. To help remember how to infuse HyQvia, we use Hy5, like the Hy in both HyQvia and hyaluronidase, this little vial.
Hy5 is the 5 steps to infuse HyQvia.
Get ready, prepare hyaluronidase or HY, prepare the immune globulin or IG, infuse HyQvia, and finish up.
Nurse: Oh, good. Your vials are at room temperature, just like they should be before you infuse HyQvia. Vials can be stored in the refrigerator or at room temperature, just remember that once you take the vials out of the refrigerator, you shouldn’t put them back in.
Nurse: They do last longer if they’re refrigerated. But, if they’ve been refrigerated, the HyQvia may take up to 60 minutes when taken out of the boxes to get to room temperature. Just something to remember to help you plan when you’ll infuse.
Nurse: Always let it come to room temperature naturally. So, don’t ever shake it, apply heat or place it in the microwave.
Patient: Got it.
Nurse: Before we dig in, let’s take a look at your vials.
Nurse: You always want to make sure they’re the correct dose, what your doctor prescribed for you.
Nurse: Check the expiration date and make sure they’re not expired. Don’t ever use them if they’re past the expiration date or if the purple cap is missing or broken. You want to handle them normally. So, no shaking. Look at the color. The Hy should be clear and colorless. And the IG should be clear and colorless, or it may be pale yellow. That’s OK. Neither should be cloudy or have any floating particles.
Patient: OK, these look OK, right?
Nurse: Yep! They look good to me. We just need to finish gathering our supplies, and clean our work area. Then we’ll program the infusion pump if needed, wash our hands, and we’re ready to move on.
Nurse: OK, let’s wash our hands and we’re ready for Hy2 of Hy5: Preparing the Hy.
Patient: OK, sounds good. The sink’s right over here.
Nurse: Now when we say “Hy”, we’re talking about the recombinant human hyaluronidase.
Nurse: Hyaluronidase is always first, so it’s infused before the IG, and Hy allows more IG to be absorbed into your body. It does this because it’s infused subcutaneously, meaning just under your skin, which allows a larger amount of IG to be absorbed into the bloodstream in one to three sites.
Nurse: So, remove the purple protective cap and ensure the blue vial caps are removed. If not, manually remove the blue caps. To prepare the Hy, without shaking the vials, first wipe them with an alcohol swab and give it 30 seconds to dry.
Nurse: Next, remove a sterile syringe from its package and attach it to the needle or needle-less transfer device.
Nurse: Next, remove the cap on the needle or needle-less transfer device and pull back on the plunger to fill the syringe with air. The amount of air should equal the amount of Hy in the vial.
Nurse: Then, insert the needle or needle-less transfer device into the center of the Hy vial stopper and push the air into the vial.
Nurse: Now, turn the vial upside down and pull back on the plunger to withdraw all of the Hy into the syringe.
Patient: Like this?
Nurse: Yes, you’ve got it.
Nurse: Now, remove the needle or needle-less transfer device from the Hy vial.
Place the cap back on the needle or needle-less transfer device.
If you have multiple Hy vials, you would repeat the previous steps for each Hy vial, using the same syringe, if possible.
Nurse: Great! So, we’ve got all the Hy we need into the syringe.
First thing we’ll want to do is hold the syringe upright and tap it to remove air bubbles. Slowly push the plunger until the Hy reaches the tip of the barrel.
Hy can also be infused manually, but we’re going to use a pump.
Clean the upper port of the pump tubing with an alcohol swab and allow to dry for approximately 30 seconds.
Remove the cap from the syringe and discard it.
Attach the syringe to the upper port of the pump administration tubing.
Then remove the cap from the subcutaneous needle set and attach it to the opposite end of the pump administration tubing.
Close the clamp on the pump administration tubing closest to the needle set.
Nurse: Hold the syringe straight up and remove the air from the pump administration tubing between the upper port and the spike. Keep the syringe upright.
Push the plunger to fill the pump tubing between the upper port and the spike. Close the clamp above the upper port. Open the clamp on the lower port.
Slowly push the plunger of the syringe to remove the air. The syringe size may vary due to a larger volume. Fill the rest of the pump administration tubing up to the needle wings with hyaluronidase. Like this. See?
Patient: Yep. Got it.
Nurse: Lay the syringe and pump administration tubing down on the clean work surface. Close the clamp or clamps on the needle set tubing.
Guess what? You’re already to Hy3.
Patient: OK!
Nurse: If using the push method to deliver Hy, transfer into the syringe or syringes, preferably using a needle-less transfer device.
Attach the syringe filled with hyaluronidase to the needle set.
Push the plunger of the syringe to remove the air and fill the needle set up to the wings with hyaluronidase.
Nurse: Hy3 is preparing the IG. First, clean each IG vial by wiping the stopper with an alcohol swab and give it 30 seconds to dry, making sure not to shake the vials as you wipe.
Nurse: OK, now tighten the connection between the pooling bag and the gravity fill set tubing.
Now take the pooling bag and pinch the white clamps to close off all the tubes that are coming out of the pooling bag. Open the package of the sterile cap and make sure to keep this little cap nearby. Here, it’s in sterile packaging. You would then want to keep it on a sterile and clean surface. OK, do you see where the pooling bag connects to the tubes? That’s the port.
Patient: Yes, this little white piece?
Nurse: Yep, right there. You want to make sure that’s tight because sometimes it can become loose in the packaging. You may want to have your caregiver or friend help you with this.
Patient: Got it. It’s tight.
Nurse: Now, remove the cap from the spike on the gravity fill set tubing—we sometimes call these tubes legs.
Nurse: Insert the spike straight down into the center of the IG vial stopper.
The tip of the spike should be all the way inside the vial.
Patient: OK, it is now.
Nurse: Great! Now turn the IG vial upside down, unclamp on the gravity fill set tubing and then open the vent on the spike. You may need to gently flick the gravity fill set tubing to float air bubbles to the top of the vial.
Patient: Like this?
Nurse: Exactly!
Nurse: Keep holding the IG vial upside down and transfer the IG into the pooling bag. Gently wiggle the spike back and forth to make sure you transfer all the IG from the vial.
Once all of the IG has been transferred, close the clamp and the vent on the gravity fill set tubing. Remove the spike from the IG vial.
If you have multiple IG vials to achieve the desired dose, you would repeat the previous steps for each IG vial, using the same pooling bag.
When you finish with the last vial, hold the gravity fill set tubing upright with the spike in the air.
Nurse: Open the clamp and tap the gravity fill set tubing to get the last drops of IG into the pooling bag.
Patient: Whoa, OK, I was with you up right until when you talked about when I’m finished with the last vial.
Nurse: That was a lot. No worries. OK, once the last vial is finished, you want to hold the pooling bag tubing upright. Tap the pooling bag tubing to get the last drops of IG into the pooling bag.
Patient: OK, got it.
Nurse: Good. Hold the pooling bag so the tubes are coming out of the top and then detach the pooling bag tubes, or legs from the pooling bag.
Patient: Is this right?
Nurse: Just like that! Next, detach the gravity fill set tubing from the pooling bag. Gently push air out of the pooling bag through the fill port. Cap the end of the fill port and close the clamp on the fill port.
Nurse: Remove the tab from the administration port of the pooling bag.
If you wanted to, you could also spike the IG vial directly using the vented pump administration tubing.
Nurse: Now, remove the protective cap from the spike on the pump administration tubing.
Nurse: Insert the spike into the administration port of the pooling bag. Hang the pooling bag onto an IV pole. Then, insert the pump administration tubing into the pump.
Nurse: If using syringes, first attach a sterile syringe to a vented spike. Then insert the vented spike into the center of the IG vials.
Next, turn the vial upside down and pull back on the plunger to pull the IG into the syringe. Repeat these steps if you are using multiple vials, to achieve the desired dose.
If using a sterile needle, attach a sterile syringe to the sterile needle and pull back the plunger of the syringe to fill with air, which should equal the amount of the liquid you will be taking from the vial.
Then insert the needle into the center of the vial and inject air in. Finally, pull back on the plunger to withdraw the desired volume.
Nurse: OK, so now we’ve prepared both the Hy and IG. Ready to infuse your HyQvia?
Patient: I am.
Nurse: Yes, that’s the attitude I’m talkin’ about.
Nurse: On to Hy4: Infusing HyQvia. The Hy and the IG will be infused the same way.
Nurse: We’ll use the infusion pump to infuse the Hy first, then the IG. Always in that order. Remember, Hy before IG.
Patient: Yes, I’ll remember.
Nurse: OK, we’ll start by choosing an infusion site. Any ideas?
Patient: Well…I’m…not exactly sure. I was kind of confused about that. Where should I?
Nurse: Totally fine. And I can help with that. You’ve got a couple of options. You can infuse in either thigh or either side of your middle to upper abdomen. And the area or place you want to infuse in can change over time after you’ve infused a few times and realized one area is more comfortable for you than another.
Patient: I think I’d like my upper abdomen.
Nurse: That will work! Remember to rotate your sites for each infusion, too. Also, most patients will need to infuse at two sites to help spread out the volume across the abdomen. This potentially allows a faster infusion time than if just one site is used. If a second site is used, you want to select sites on the opposite sides of your body and infuse half the total volume of Hy in each site. If using three sites, the sites should be 4 inches or 10 centimeters apart. And be sure to rotate sites by choosing opposite sides of the body between your infusions.
Nurse: OK, use a new alcohol swab to clean your abdomen, beginning at the center of each infusion site and moving outward in a circular motion. Be sure to let it dry completely—about 30 seconds.
Good.
Nurse: Now, I want to make sure I mention a few things about the needles. You want to avoid any bony areas, blood vessels, scars, and any areas of inflammation, irritation, or infection.
Your goal is to insert the needle just under the skin, into the fatty layer. Now, if the needle is too short, you may experience a burning sensation or leakage, but, on the other hand, if it’s too long, you’ll reach the muscle layer, and you don’t want to do that because it could be painful. If you feel that you need a needle of a different length, speak with your doctor and reach out to your specialty pharmacy, because that’s where you can get the new needle or needles.
Nurse: Remove the needle cap and firmly grasp and pinch at least one inch of skin between two fingers. Insert the 24-gauge subcutaneous needle with a rapid motion straight into your skin at a 90-degree angle. Alright, you just gotta do it!
Nurse: Yes! Just like that. You did it. You OK?
Patient: Surprisingly, yes.
Nurse: You did great. Now, secure the needle in place with the sterile tape.
Close the clamp above the lower port of the pump administration tubing.
Clean the lower port with an alcohol swab and allow to dry for at least 30 seconds.
Nurse: Great. Ready to start?
Patient: Well, I’ve come this far. Let’s do it.
Nurse: OK, here we go!
Attach a 5-milliliter syringe to the lower port. Open the needle set tubing and gently pull back on the syringe plunger. Look for blood return in the tubing. If there’s no blood, remove the syringe keeping the needle in place. Secure the needle set by applying a sterile, clear dressing over the site. If more than one infusion site is needed, you'll follow these steps to check for proper needle placement in all sites at the same time.
Nurse: If blood is seen in the tubing, remove and discard the needle and start at a new site with a new subcutaneous needle.
Check to make sure the clamp above the lower port is open.
Then, insert the pump administration tubing into the pump.
Nurse: To infuse the Hy, first turn on the pump. Your specialty pharmacy will have already pre-programmed it for you—in this case, sixty to one hundred twenty milliliters per hour per infusion site and increase it as you can tolerate it, whatever you feel comfortable with.
When the syringe is empty, the pump will say that there is an occlusion alarm. Right here.
Patient: I see that.
Nurse: OK, so now pause the pump and remove the empty syringe. Next, open the clamp above the upper port and restart the pump. The IG will then help to push the Hy into the infusion sites. Now, if more than 1 site is used, divide the IG equally between sites.
Patient: Ah, OK.
Nurse: Now, make sure to start the IG infusion within 10 minutes of completing the infusion of Hy.
Nurse: I’m sure at some point you’ve heard or read about ramping up, right?
Patient: Yes, my doctor talked to me about it. She said I’d start at a lower volume and increase over several infusions.
Nurse: That’s exactly right. It’s a way to help your body adjust to your new medicine.
Nurse: So when the IG infusion is complete, flush any remaining IG from the pump administration tubing with saline to ensure that you receive your full dose. To do that, first remove the pump tubing spike from the pooling bag administration port. Then, pull the tab off the saline bag administration port and insert the pump tubing spike into the administration port. Finally, restart the pump to flush the remaining IG from the pump tubing.
Nurse: So the whole infusion time of Hy followed by IG typically takes about 2 hours if the dose of HyQvia is being infused monthly, but as far as setting up your infusion goes, that’s a wrap! You did it.
Patient: You mean that’s it?
Nurse: For the infusion, yes.
Nurse: We’re at Hy5: Finish up.
Nurse: You’re going to loosen all the edges of the dressing and pull the needle wings straight up and out. Place a bandage over the infusion site. Then, dispose of the needle set in the sharps container.
Nurse: I do have to say that patients typically experience swelling at the infusion site. People call it a “pancake” because your skin swells in the shape of a pancake. However, it is common and nothing to panic about. This means the Hy is doing what it’s supposed to do. It will go down, usually in one to three days, and it occurs because of the volume of fluid infused. Contact your doctor though if an infusion site reaction increases in severity or lasts more than a few days.
Patient: That sounds a little weird, but I’m definitely glad you told me about it, so I know what to expect.
Nurse: I know it does, but I want you to know and not be surprised when it happens. It’s common.
Nurse: Other than that, you may experience infusion site reactions, local reactions, like mild or moderate pain, redness, swelling, and itching at the infusion site. The most common side effects are headache, fatigue, nausea, fever, itching, redness, abdominal pain, back pain, and pain in extremity. Keep in mind these are not all the possible side effects of HyQvia. Talk to your doctor about any side effects that bother you or don’t go away.
Nurse: I’m sure you’ve heard or read about side effects, but just making sure we go over them too. You’ll want to contact your doctor if any reaction concerns you or doesn’t go away.
Nurse: Now, you’ll want to record your infusion details in your Wellness Journal. You’ll want to write down the date, time, dose, and infusion site or sites to assist in rotating sites and any reactions after each infusion. A trick for your Wellness Journal, most patients just pull the labels right off their IG vials, which have the product lot number, vial size, and expiration date, and put them in their journal.
There’s even space to write down questions and thoughts, like how long a certain step took or just notes about remembering what to do. It’s a good place to write down any questions you may have for your healthcare team as well.
Nurse: You did it! You just learned how to use Hy5 as a way to help remember how to infuse HyQvia. Seriously, you did great. I hope you’re proud of yourself.
Patient: I am. I was so nervous, but I think I can do this. Thank you so much.
Nurse: Of course! I know you’ve got this. You can have more training, until you and your healthcare team feel comfortable with self-infusing HyQvia. You also have resources to rely on, should you need them. And, if you have questions about anything, talk to your doctor. You can also visit HyQvia.com. Remember to use the patient log in your wellness journal to keep track of your infusions.
Patient: Yeah, I will.
Nurse: Now, I’ll help you gather this stuff up so it’s ready to go next time, and then you take it easy the rest of the day.
Patient: Thanks!
Please stay tuned to the remainder of this video for additional Important Safety Information.
Nurse: What is HyQvia?
HyQvia is a liquid medicine that is given under the skin (subcutaneously) to treat chronic inflammatory demyelinating polyneuropathy (CIDP) in adults.
IMPORTANT SAFETY INFORMATION
What is the most important information that I should know about HyQvia?
- HyQvia can cause blood clots.
- Call your healthcare professional (HCP) if you have pain, swelling, warmth, redness, or a lump in your legs or arms, other than at the infusion site(s), unexplained shortness of breath, chest pain or discomfort that worsens on deep breathing, unexplained rapid pulse, numbness or weakness on one side of the body.
- Your HCP may perform blood tests regularly to check your IgG level.
- Do not infuse HyQvia into or around an infected or red swollen area because it can cause infection to spread.
Nurse: Who should not take HyQvia?
Do not take HyQvia if you:
- Are allergic to IgG, hyaluronidase, other blood products, or any ingredient in HyQvia.
Nurse: What should I avoid while taking HyQvia?
- HyQvia can make vaccines (like measles/mumps/rubella or chickenpox vaccines) not work as well for you. Before you get any vaccines, tell your HCP that you take HyQvia.
What should I tell my HCP before I start using or while using HyQvia? Tell your HCP if you:
- Have or had any kidney, liver, or heart problems or history of blood clots because HyQvia can make these problems worse.
- Have IgA deficiency or a history of severe allergic reactions to IgG or other blood products.
- Are pregnant, trying to become pregnant or are breast feeding. It is not known whether HyQvia can harm the unborn baby or breastfed infant.
Nurse: What are the possible or reasonably likely side effects of HyQvia?
HyQvia can cause serious side effects. If any of the following problems occur after starting HyQvia, stop the infusion immediately and contact your HCP or call emergency services:
- Hives, swelling in the mouth or throat, itching, trouble breathing, wheezing, fainting or dizziness. These could be signs of a serious allergic reaction.
- Bad headache with nausea, vomiting, stiff neck, fever, and sensitivity to light. These could be signs of irritation and swelling of the lining around your brain.
- Reduced urination, sudden weight gain, or swelling in your legs. These could be signs of a kidney problem.
- Pain, swelling, warmth, redness, or a lump in your legs or arms, other than at the infusion site(s). These could be signs of a blood clot.
- Brown or red urine, fast heart rate, yellow skin or eyes. These could be signs of a liver or blood problem.
- Chest pain or trouble breathing, blue lips or extremities. These could be signs of a serious heart or lung problem.
- Fever over 100°F. This could be a sign of an infection.
Nurse: After HyQvia infusion a temporary, soft swelling may occur around the infusion site, which may last 1 to 3 days, due to the volume of fluid infused.
The following possible side effects may occur at the site of infusion and generally go away within a few hours, and are less likely after the first few infusions.
- Mild or moderate pain
- Redness
- Swelling
- Itching
Nurse: The most common side effects of HyQvia are:
- Headache
- Fatigue
- Nausea
- Fever
- Itching
- Redness
- Abdominal pain
- Back pain
- Pain in extremity
Antibodies to the hyaluronidase component of HyQvia were formed in some patients taking HyQvia. It is not known if there is any long-term effect. In theory, these antibodies could react with your body’s own hyaluronidase (PH20). PH20 is present in the male reproductive tract. So far, these antibodies have not been associated with increased or new side-effects.
Nurse: These are not all the possible side effects. Talk to your HCP about any side effect that bothers you or that does not go away.
Nurse: Please see Important Safety Information throughout this video, and accompanying Information for Patients, including Warning about Blood Clots, or visit www.hyqvia.com/information-for-patients.
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch, or call 1-800-FDA-1088.
Nurse: This video is intended for patients 17 years of age or older taking HyQvia. HyQvia is for patients two years and older with either primary immunodeficiency, PI, or adult patients with chronic inflammatory demyelinating polyneuropathy, CIDP. If you have PI, it does not mean you have CIDP. And if you have CIDP, it does not mean you have PI.
Nurse: HyHub and HyHub Duo important information for patients. What is HyHub and HyHub Duo? HyHub and HyHub Duo are stand-alone, single use, disposable vial access devices. Who should use HyHub and HyHub Duo? HyHub and HyHub Duo are for patients 17 years of age and older to allow HyQvia, Immune Globulin Infusion, human, 10% with Recombinant Human Hyaluronidase, to be transferred from vials without using a needle as prescribed in a home environment or clinical setting.
Nurse: Do not use HyHub and HyHub Duo with a pooling bag. Do not connect HyHub and HyHub Duo to a syringe driver infusion pump. Selected information for patients. HyHub and HyHub Duo are for single use only, even if all docks are not used during a single infusion. Reuse will increase risk of infection. Always use a new HyHub and HyHub Duo for each infusion.
Nurse: Only use HyHub and HyHub Duo when ready to administer HyQvia. Do not use HyHub and HyHub Duo at home until receiving instructions and training from a healthcare provider. HyQvia is the only medicine that may be used with HyHub and HyHub Duo. Do not exceed the maximum infusion volume per infusion site or infusion rate as indicated in the HyQvia prescribing information or as directed by a healthcare provider.
Nurse: For safe and proper use of HyHub and HyHub Duo, please refer to the complete instructions for use included with the devices. Talk to your healthcare provider if you have additional questions. For information about HyQvia, including warnings for blood clots, please see Patient Information for HyQvia. What is HyQvia?
Nurse: HyQvia is a liquid medicine that is given under the skin, subcutaneously, to treat primary immunodeficiency, PI, in people two years and older, and Chronic Inflammatory Demyelinating Polyneuropathy, CIDP, in adults. Important safety information. What is the most important information that I should know about HyQvia? HyQvia can cause blood clots.
Nurse: Call your healthcare professional, HCP, if you have pain, swelling, warmth, redness, or a lump in your legs or arms, other than at the infusion sites, unexplained shortness of breath, chest pain or discomfort that worsens on deep breathing, unexplained rapid pulse, numbness, or weakness on one side of the body. Your HCP may perform blood tests regularly to check your IgG level. Do not infuse HyQvia into or around an infected or red, swollen area because it can cause infection to spread. Please see additional important safety information within this video.
Nurse: Accompanying information for patients can be found on HyQvia.com. If you have questions about HyQvia, contact your doctor. For questions about HyHub or HyHub Duo, contact your healthcare provider, which may include your specialty pharmacy.
Nurse: Remember, you must receive appropriate training before you're able to infuse at home by yourself. If you are an existing HyQvia patient who has received prior training, you will also require additional training if you and your HCP determine that infusing with HyHub is right for you. If you have a friend or caregiver who helps you infuse, they will follow the same steps in the exact same way.
Nurse: Please note that the instructions shown in this video are the same for both HyHub, which holds up to four dual-vial units, and HyHub Duo, which holds up to two dual-vial units. We'll be using the four-dock tray for this training. Hi, I'm Kristina, and I'm a nurse. I'm here to teach you how to use the HyHub infusion tray at home, designed to help to simplify the infusion process without use of transfer needles.
Nurse: The HyHub tray allows you to infuse without a pooling bag and cuts down on the number of steps required to prepare hy and IG when using two, three, or four dual-vial units. Don't worry, I'll go over it all and explain the HyHub infusion process. Let's get started. If you're already a HyQvia patient, some of these steps might feel familiar.
Nurse: However, it's still important to watch this video so you know exactly what to do when infusing with HyHub. If you have received your box of supplies, you might want to have it with you as you watch this video. In addition, there is a step-by-step guide available online in case you'd like to use it as a reference.
Nurse: To help with the training process, we've broken the infusion process down to five steps. We call them hy1, hy2, all the way to hy5, the perfect way to end an infusion. Hy5 is also what we call the whole infusion process. We start the process at hy1, checking the HyHub infusion tray and vials, gathering all the supplies, and preparing for infusion.
Nurse: Do not begin the infusion procedure until you have all required supplies and you are ready to administer your prescribed medication. First, you'll need to clean the surface where you'll be infusing with antibacterial cleaner. Once clean, open the HyHub box and take out the HyHub infusion tray, which should be right on top. The HyHub infusion tray is the device that helps to simplify the infusion process without use of transfer needles.
Nurse: Let's look at what else is in the box and take a few minutes to get you familiar with the supplies. Here is your hyaluronidase, or hy, and your IG vials. The size and number of the vials may vary depending on the dose you've been prescribed. This is your pump. And here is your pump tubing. Here's the syringe and subcutaneous needle set.
Nurse: Then here's your sharps container. This is where you dispose of the needle set when you're done. We'll get to that at the end of the infusion. The rest of the box should contain gloves, a prefilled saline syringe, or dextrose 5% in water, tape, a bandage, gauze, and alcohol swabs to clean the tops of your vials and your body where you infuse.
Nurse: And last but not least, here is your wellness journal. This is where you keep track of your treatments, any reactions after each infusion, and write down your thoughts for yourself or questions for your doctor. If you did not receive a wellness journal in your shipment and would like one, you can request one through Takeda Patient Support if you are a PI patient, or order one through HyQvia.com if you're a CIDP patient.
Nurse: If this feels different than what you're used to, I get it. Once you learn what's what, infusing with HyHub will help simplify the process without the use of transfer needles. And remember, there are a few ways to get more information. There's a step-by-step guide that outlines the steps in an easy-to-use format, and your healthcare provider, which may include your specialty pharmacy, is also an excellent resource if you have questions.
Nurse: Your infusion mat also has a QR code linking to this video if you ever want a refresher. Let's begin. First, be sure that the infusion pump is programmed according to your prescribed infusion rate and the manufacturer instructions. If using more than one infusion site, do not exceed pump infusion rate of 600 milliliters per hour.
Nurse: For example, 300 milliliters per hour per site for two sites or 200 milliliters per hour per site for three sites. Whenever you do an infusion, it's important to remember that the hy comes before the IG, or immune globulin infusion. To help yourself remember, try saying "hi" before IG. It's just like starting a conversation. You always start with "hi." I tell people to start with "hi" even when they are laying things out just so they can remember.
Nurse: Make sure your vials are room temperature by leaving them out for about an hour. Never apply heat or put your vials in the microwave to warm them up. You always want the medication to come to room temperature naturally. Also be sure to check the expiration dates on your vials. Don't use your vials if the expiration date has passed or if the purple protective cap is missing or broken.
Nurse: If you observe any expired or damaged materials, contact your doctor as soon as possible. Next, you always want to confirm you have the correct dose, which is what your doctor prescribed for you. Now, look at the labels on the vials. The small dual-vial is recombinant human hyaluronidase. We call that hy for short. The larger one is immunoglobulin 10%, or IG for short.
Nurse: You want to handle them carefully, so don't shake the vials. Look at the color. The hy should be clear and colorless and the IG should be clear and colorless, or it may be pale yellow. That's okay. Neither should be cloudy or have any floating particles. Now you'll want to wash your hands thoroughly with soap and let them dry.
Nurse: Wearing gloves is optional, but you should wear them if that's what has been recommended by your doctor. Before we go any further, let's look at the HyHub infusion tray in its packaging. You want to check the expiration date, which is located right on the packaging. Never use an expired HyHub tray or other expired infusion materials. Open and inspect the supply packaging.
Nurse: You don't ever want to use HyHub if its sterile packaging or components appear to be broken, missing, or expired. That may cause infection, leaks from the product, or other hazardous conditions that could result in serious injury. If observed, contact your healthcare provider, which may include your specialty pharmacy. You'll notice HyHub is numbered and color-coded to help with following the instructions.
Nurse: The tubing is built inside, and these are the hy and IG connectors which will be used to transfer the medication from the vials. The purple hy connector connects to the syringe to pool hy from all dual-vial units docked into HyHub. The orange IG connector connects to the pump tubing to deliver IG from all dual-vial units docked into HyHub.
Nurse: This is where your vials dock in. You'll push them down and lock them into place. Next, remove the purple caps from both dual-vial units. This should make the blue caps underneath pop right off. If they don't, remove them manually. You'll need to clean the tops of all the vials using a separate alcohol swab for each, and give them 30 seconds to dry.
Nurse: Start with the hy vials and then do the IG vials. Now that they're clean, dock the vials into the HyHub infusion tray. See the numbers on the covers? That's to show the order for adding the vials. You can add up to four dual-vial units, but as you can see, we only use two in this example.
Nurse: Keep in mind, HyHub Duo has two docks and can hold up to two DVUs. The following steps will be the same for each set of vials, whether you are using one, two, three, or four. If you use more than four dual-vial units per infusion, please contact your healthcare professional for instructions. No matter how many you need to use, adding them to the HyHub infusion tray is the same.
Nurse: Remove the cover, being careful not to touch or remove anything under it. Touching anything under the cover will increase the risk of contamination and interfere with the normal function of HyHub. Insert the vials into dock one with the stoppers facing down. Push down so that the vials lock into place. You may hear a click, which is an indicator that the dual-vial unit is locked in place.
Nurse: Once the vials have been locked into place, don't try to remove them from the dock. Don't rotate the vials after docking either. This may cause leaks or damage to the spikes. And notice which vial is at the front? Hy before IG. It is important to insert the DVUs in the order of the dock numbers.
Nurse: If using more than one dual-vial unit, repeat docking steps for the remaining dual-vial units and insert them in order into docks two, three, and four as needed. Depending on the infusion dose and number of dual-vial units, you may not use all docks. Next, you're going to remove the syringe from the packaging and attach the syringe to the hy connector on the HyHub infusion tray.
Nurse: The hy connector is this purple piece right here. You never want to touch the tip of the hy connector because you don't want to accidentally contaminate it. Now go ahead and pull it gently away from the infusion tray. That will reveal the tubing. Before connecting the syringe to the hy connector, make sure to remove all the air from the syringe by pushing down on the syringe plunger.
Nurse: Now attach the syringe to the end of the purple hy connector by pushing in and twisting the syringe onto the hy connector. It's time to slowly pull back on the syringe's plunger to draw all the hy up into the syringe. Do not push any air into your HyHub. Remove the syringe from the hy connector with a twist to the left.
Nurse: More than one syringe may be needed to administer your complete dose, depending on the total volume of your infusion. Now that you've got all the hy you need into the syringe, point the syringe tip up and push the syringe's plunger up to remove air. Next, you'll attach the syringe to the needle set. To do this, remove the cap from the end of the needle set tubing.
Nurse: Twist the syringe filled with hy onto the tubing connected to the end of the needle set. Fill the needle set tubing with hy until it reaches the needle wings. Don't push the hy beyond the needle wings. At this point, you'll attach the pump tubing to the IG connector on the HyHub infusion tray. That's this orange piece right here.
Nurse: You'll twist the pump tubing onto the IG connector to log it in place. But remember, you never want to touch the tip of the IG connector because you don't want to accidentally increase the risk of contamination and infection. Once it's in there nice and tight, insert the pump tubing into the pump itself. The top flips open and the tubing fits right in here.
Nurse: Go ahead and put the tubing in and fill it according to the pump manufacturer's instructions. When using HyHub, you will need to add one milliliter to your IG filling volume. Great, you're ready for hy2, prepare the infusion site. You'll need to decide where you want to infuse, either in your middle to upper abdomen or thighs.
Nurse: Avoid bony areas like the ribs, visible blood vessels, scars, and any areas of inflammation or infection. Remember to rotate your sites for each infusion by choosing opposite sides of the body between future infusions. If your doctor tells you to infuse in two sites, select sites on opposite sides of the body. If you have a wellness journal, write down your infusion sites. If you don't have a journal, use a dedicated notebook to record your infusion sites.
Nurse: Use a new alcohol swab to clean your abdomen and allow it to dry at least 30 seconds. If you're using more than one infusion site, you will need to follow these steps again. Okay, we're at hy3, infuse hy. Now that you've prepared the infusion site, remove the needle cover and then firmly grasp and pinch at least one inch of skin between two fingers.
Nurse: Hold the needle set so that the needle is pointed at a 90-degree angle straight at where you want it to go in. Insert the needle with a rapid motion straight into your skin. Use some of the sterile tape to secure the needle in place. You'll want to repeat these steps if you're using more than one infusion site.
Nurse: Now, let's do a needle check with the syringe filled with hy to make sure the placement is good. Pull back on the syringe's plunger to check for blood return in the tubing of the needle set. If you see blood in the tubing, remove and discard the subcutaneous needle and repeat hy2 and hy3 with a new subcutaneous needle and infusion site.
Nurse: Secure the needle set by applying a sterile clear dressing. You want to infuse the hy manually at an initial rate per infusion site of approximately one to two milliliters per minute and increase as tolerated. If you're using more than one infusion site, divide the hy equally between sites. After infusing all the contents in the syringe, remove the empty hy syringe from the needle set.
Nurse: Remove the sterile cap on the pump tubing and twist the pump tubing filled with IG to the right onto the same needle set. You're ready to infuse IG. This is hy4. HyHub usually comes with a peristaltic pump. You want to make sure the pump tubing is properly secured to the needle set within 10 minutes of completing the infusion of hy.
Nurse: Start the pump to infuse the IG from all docked IG vials. Your pump will make a little humming sound. That's good. It means it's working. Never rotate the vials during the infusion. This may cause leaking or damage to the spikes. And be sure to keep the HyHub infusion tray level during infusion to prevent air from entering the system.
Nurse: You may notice a soft, wide swollen area around your infusion site due to the amount of fluid you infused. This is normal. If you have trouble with any swelling or pain, it is recommended to use a warm or cold compress, but do not leave it on for more than 10 minutes at a time. The swelling should go away after one to three days, but if it doesn't or begins to worsen, call your doctor.
Nurse: Other than that, you may experience mild or moderate pain, redness, swelling, and itching at the infusion site. The most common general side effects are headache, vomiting, fatigue, nausea, and fever. Remember, these are not all the possible side effects. You'll want to contact your doctor if a reaction concerns you or does not go away. This takes us to hy5.
Nurse: Complete the infusion and dispose of the infusion set and HyHub. At the end of the infusion, check to ensure all the medicine has been infused from the IG vial. If medicine remains, resume the infusion until the entire dose of IG has been infused. Next, remove the IG connector from the pump tubing. This next step is optional, but you can flush the tubing if directed to do so by your doctor.
Nurse: You do this by twisting a prefilled flush syringe of saline, approximately five milliliters, onto the tubing. Push the syringe's plunger to receive the entire IG dose prescribed. Remove the needle set by loosening the tape on all edges. Pull the needle wings straight up and out. Gently press a small piece of gauze over the infusion site and cover with a bandage.
Nurse: After removing the needle or needles from your skin, you will discard the infusion set, including the tray with the vials attached and all the other disposable supplies as directed by your doctor in accordance with local requirements. And remember, the HyHub infusion tray is for single use only. You will receive a new one for each infusion with your prescription, which you will use and dispose of as directed.
Nurse: You can't re-sterilize the tray. Reuse will increase your risk of infection. This is really important. The last thing is to record the infusion details in your wellness journal if you have one. Look at the batch numbers on the vials and write those in, as well as the date and time, sites of infusion, any reactions after each infusion, and any notes you want to remember or experiences you want to talk about with your treatment team.
Nurse: You can peel your labels off your vials and place them in your wellness journal or dedicated infusion notebook as well. Congratulations, you're done. That's the hy5. Don't forget, if you have questions about HyQvia, talk to your doctor. If you have questions about HyHub or HyHub Duo and the infusion process, contact your healthcare provider, which may include your specialty pharmacy.
Nurse: You can also visit HyQvia.com. What is HyQvia? HyQvia is a liquid medicine that is given under the skin, subcutaneously, to treat primary immunodeficiency, PI, in people two years and older, and Chronic Inflammatory Demyelinating Polyneuropathy, CIDP, in adults. Important safety information. What is the most important information that I should know about HyQvia? HyQvia can cause blood clots.
Nurse: Call your healthcare professional, HCP, if you have pain, swelling, warmth, redness, or a lump in your legs or arms, other than at the infusion sites, unexplained shortness of breath, chest pain or discomfort that worsens on deep breathing, unexplained rapid pulse, numbness, or weakness on one side of the body. Your HCP may perform blood tests regularly to check your IG level.
Nurse: Do not infuse HyQvia into or around an infected or red, swollen area because it can cause infection to spread. Who should not take HyQvia? Do not take HyQvia if you are allergic to IgG, hyaluronidase, other blood products, or any ingredient in HyQvia. What should I avoid while taking HyQvia? HyQvia can make vaccines like measles, mumps, rubella, or chickenpox vaccines not work as well for you.
Nurse: Before you get any vaccines, tell your HCP that you take HyQvia. What should I tell my HCP before I start using or while using HyQvia? Tell your HCP if you have or had any kidney, liver, or heart problems or history of blood clots because HyQvia can make these problems worse.
Nurse: If you have IgA deficiency or a history of severe allergic reactions to IgG or other blood products, if you are pregnant, trying to become pregnant, or are breastfeeding. It is not known whether HyQvia can harm the unborn baby or breastfed infant. What are the possible or reasonably likely side effects of HyQvia? HyQvia can cause serious side effects. If any of the following problems occur after starting HyQvia, stop the infusion immediately and contact your HCP or call emergency services.
Nurse: Hives, swelling in the mouth or throat, itching, trouble breathing, wheezing, fainting, or dizziness. These could be signs of a serious allergic reaction. Bad headache with nausea, vomiting, stiff neck, fever, and sensitivity to light. These could be signs of irritation and swelling of the lining around your brain. Reduced urination, sudden weight gain, or swelling in your legs.
Nurse: These could be signs of a kidney problem. Pain, swelling, warmth, redness, or a lump in your legs or arms, other than at the infusion sites. These could be signs of a blood clot. Brown or red urine, fast heart rate, yellow skin or eyes. These could be signs of a liver or blood problem. Chest pain or trouble breathing, blue lips or extremities.
Nurse: These could be signs of a serious heart or lung problem. Fever over 100 degrees Fahrenheit. This could be a sign of an infection. After HyQvia infusion, a temporary soft swelling may occur around the infusion site, which may last one to three days due to the volume of fluid infused. The following possible side effects may occur at the site of infusion and generally go away within a few hours and are less likely after the first few infusions.
Nurse: Mild or moderate pain, redness, swelling, itching. The most common side effects of HyQvia in PI are headache, fatigue, nausea, fever, vomiting. The most common side effects of HyQvia in CIDP are headache, fatigue, nausea, fever, itching, redness, abdominal pain, back pain, pain in extremity. Antibodies to the hyaluronidase component of HyQvia were formed in some patients taking HyQvia.
Nurse: It is not known if there is any long-term effect. In theory, these antibodies could react with your body's own hyaluronidase, PH20. PH20 is present in the male reproductive tract. So far, these antibodies have not been associated with increased or new side effects. These are not all the possible side effects. Talk to your HCP about any side effect that bothers you or that does not go away.
Nurse: Please see additional important safety information throughout this video and accompanying information for patients found on HyQvia.com and discuss with your healthcare provider. You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch, or call 1-800-FDA-1088.

Find safety information here.
This is where you’ll find important safety info, including a warning about blood clots, to consider when starting and monitoring your treatment with HyQvia and to discuss with your doctor.
Understanding the insurance process can make
a difference
When you are prescribed a specialty medicine like HyQvia, your doctor may be required to
reach out to your health plan to get preapproval for your treatment. Work with your doctor’s
office to ensure you know what your insurance covers and how much HyQvia will cost.
Benefits verification
The first step in the process is for your doctor’s office to do a benefits verification on your behalf. They will work with your insurance company to determine if HyQvia is covered under your health plan, how much insurance will pay, what your deductible will be, and how much you will pay out of pocket. Once the office receives this information, speak to the office manager to fully understand what you are responsible for.
Prior authorization
Next, your doctor has to show your health plan that HyQvia is the appropriate treatment for you based on your medical profile. This is called prior authorization. Documentation and relevant lab tests will be sent to the health plan, and you must be approved before further coverage is granted.
Sometimes, these processes will be managed
by a specialty pharmacy provider (SPP).
Your SPP may contact you to coordinate these steps.

Our support specialists
are never more than
a tap or call away.
1-866-861-1750, Monday through
Friday, 8 AM to 8 PM ET.
Working with your specialty pharmacy provider
to get HyQvia
HyQvia is a specialty drug, which means you can’t pick up your prescription at the local
pharmacy. SPPs carry drugs for rare conditions such as CIDP and make sure they are
stored and handled appropriately before they are shipped. Your doctor will order HyQvia
through an SPP, and it will be delivered to your preferred location.
Here’s what to expect when working with an SPP:
- SPPs are able to support you by working directly with your insurance company to find out how your health plan covers HyQvia. They can assist with steps in the approval process, such as benefits verification, prior authorization, financial assistance, and treatment education—you can expect an SPP to contact you after a physician prescribes you HyQvia
- SPPs will coordinate delivery of HyQvia. Depending on your discussion with your doctor, you will have HyQvia delivered to your home or to an infusion center. They may also give you special instructions on how to store your drug properly before you take it
- Some insurance companies may only work with certain specialty pharmacies. Currently, only the below SPPs have HyQvia in stock. Work with your doctor’s office or an insurance representative to determine which SPP is available to you
The following SPPs are currently authorized to dispense HyQvia:
AcariaHealth Specialty Pharmacy
Accredo Specialty Pharmacy
Advanced Infusion Care
AmeriPharma Specialty Care
Amerita, Inc.
AOM Infusion
Axiva Health Solutions
BioMatrix
BioPlus Specialty Pharmacy
Blue Sky
California Specialty Pharmacy
Care Fusion Rx
CenterWell Specialty Pharmacy
Chartwell Pharmacy
ContinuumRx
CSI Pharmacy
CVS Specialty
HPC Specialty Infusion
InfuCare Rx
IV Solutions Rx
KabaFusion
Maxor Specialty Pharmacy
Nufactor
Option Care Health
Optum Infusion Pharmacy
OSO Home Care Inc.
Palmetto Infusion
PromptCare
Realo Specialty Care Pharmacy
Soleo Health
Specialty Care Rx
Sunrise Rx
Superior Biologics
Upstate HomeCare
Vital Care Infusion Services
Vivo Infusion
Walgreens Specialty Pharmacy
Inquire with specific SPPs for current status.

Ready to talk to your doctor?
Great. We’ve got just the support for you. Our Doctor Discussion Guide can help you get organized and ready for your conversation with your doctor.
CIDP=chronic inflammatory demyelinating polyneuropathy; HCP=healthcare professional;
Hy=hyaluronidase; IG=immune globulin; IVIG=intravenous immune globulin.
 , and
, and